Reclaiming Chronic Pain
By reclaiming ideas around chronic pain, many of those who contend with the condition are getting their lives back.
“Anybody with chronic pain will tell you, they’ve kind of been told ‘it’s all in your head.’ Or, you’re just going to have to learn to live with it."
Lee Vaughan, who works as a leisure centre worker in Sheffield, is just one of many people in the UK who suffer with a chronic pain condition day-to-day.
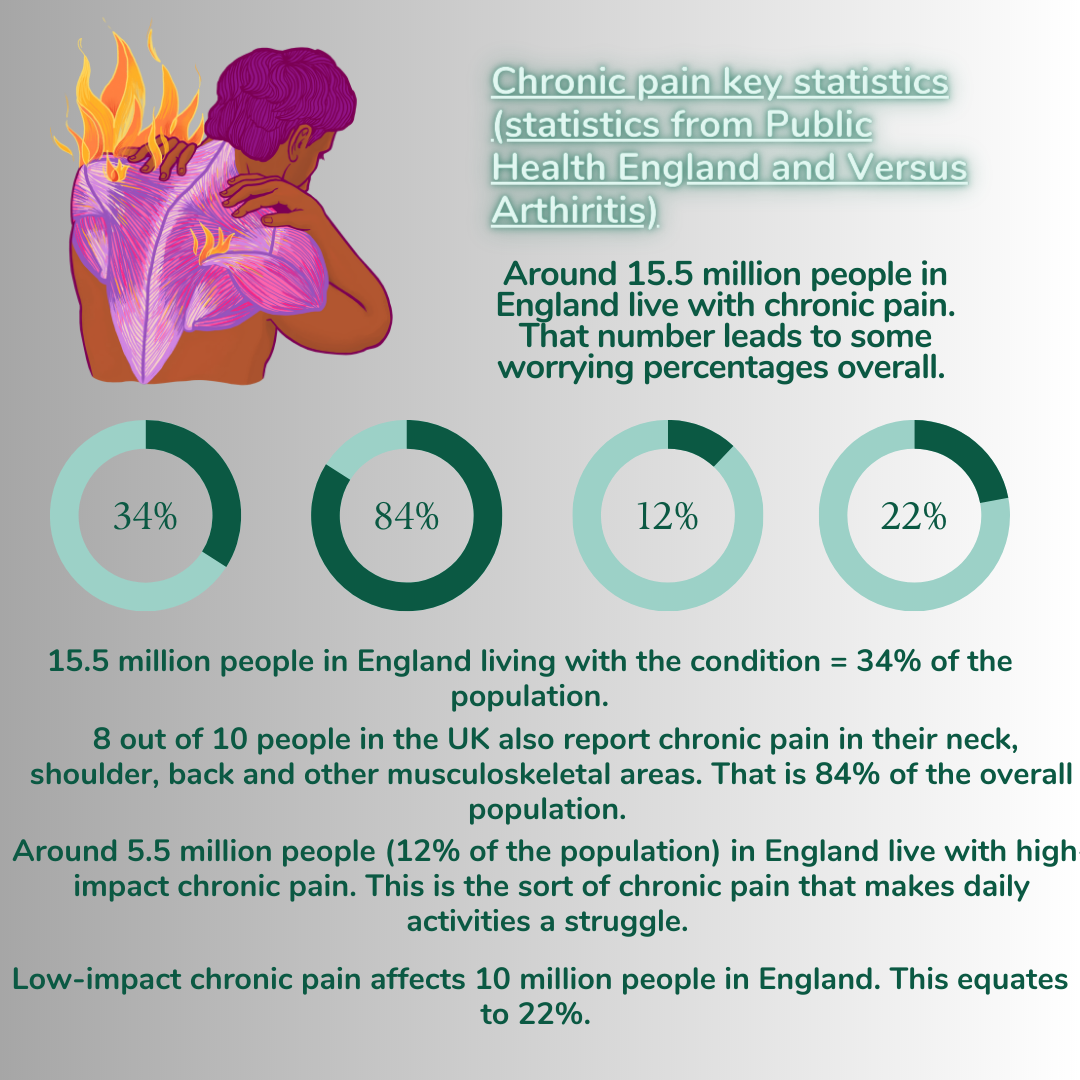
Statistics suggest, according to Public Health England from 2017, that the often overlooked condition affects 34% of the general population. This means around 15.5 million in England live with chronic pain in some capacity.
A further study conducted in February this year even suggests that chronic pain and the cognitive decline that can occur has links with dementia and Alzheimer's in later life - "People affected by multisite chronic pain may be less able to adhere to regular physical activity as one potential mechanism for increased dementia risk."
Feeling aimless about his condition, the Steel City born 49-year-old is beginning to reclaim his chronic pain by setting up support groups and more.





Lee's experience
Lee Vaughan has wrestled with the effects of chronic pain for most of his life.
His chronic pain condition was triggered by past trauma. As a child, Mr Vaughan watched his father die suddenly in his childhood home.
By the time he had turned 18, it started to have a toll on physical activities such as playing football but was always dismissed as an innocuous sports-related injury.
He said: "From about eighteen years old, my pain started to creep in. I used to be able to play football two to three times a week at that age to then take three to four days to recover. That’s not normal.
"It was always, you’ve got a groin strain, a leg injury. Anything but the actual reason. Exploring behind it didn’t exist."
Despite all this, Mr Vaughan will undergo a daring five day 300 mile bike ride across Teesside alongside 24 other cyclists in partnership with Flippin' Pain - a public health campaign attempting to change the way we think about, talk about and treat persistent pain.
Mr Vaughan himself has also started a support group in Sheffield called 'Partnering Pain'. The group helps those dealing with the condition and guides them to appropriate physical activity to stay active.
Louise's Experience
Louise Trewern, who lives in Torquay, has also begun to readdress her experiences with chronic pain.
Ms Trewern has lived with fibromyalgia for most of her life, a condition that results in an increased sensitivity to pain, muscle stiffness and many other harmful symptoms.
After years of being prescribed opioids and remaining sheltered, she's now a 'lived experience pain consultant' speaking out about how the once preferred medication method led to a 'horrid' addiction.
She said: "Opioids came into the picture when one morning, I woke up and couldn't move. I literally could not move an inch.
So, I went to the doctors, and immediately it was drugs. As we now know, you build tolerance to opioids. As time went on, the dose had to be increased.
I ended up being on them for about twelve years. So, yeah, it was pretty horrid."
Now, through speaking about her experiences and engaging in other ways to treat her pain - which includes swimming in the sea - she's living her life again.





Fiona's experience
Fiona Symington, who is now studying an MSc in health psychology at the University of Bath, has contended with chronic pain since childhood.
A fall during a horse ride left her with on and off pain in her left leg, a pain that would begin to persist.
Constant medical check-ups left her feeling directionless on her condition, with some treatments doing more bad than good.
She said: "They were traumatic treatments too. The doctors never seemed to know how to help me."
Fiona has, however, found solace in the ever-growing online chronic pain community. This has led to her studying health psychology, to help other people going through chronic pain journeys.
She said: "I joined a Facebook group for people with chronic illnesses and it was a lifeline to me.
"It changed my life to be able to talk to other people who got it."
Tim's experience
Tim Atkinson, a Lincolnshire based author, has had a chronic pain condition for 25-30 years.
He channelled his experiences into the book 'Where Does It Hurt?' - a project that initially was labelled as a 'misery memoir.'
Instead, during the writing process, it opened Mr Atkinson's eyes to new revolutionary ideas about pain management.
He said: "The work I had started to do on the so-called 'misery memoir' really just blew my mind.
"People need to challenge how they're treated, that stock phrase 'no pain, no gain' does apply in chronic pain situations."
Mr Atkinson has conquered his own arthritis this March too, taking on the March The Month challenge - his aim is to walk 11,000 steps every day during the month to raise money for Prostate Cancer UK.
"Understanding the patient journey made me realise what I need
to offer in my consultations and close the perceived gaps.
"That can often change the patient
outlook from one of despair and hopelessness to one of hope and empowerment." - Dr Deepak Ravindran.

Changing attitudes to pain
Attitudes towards pain are certainly changing, for the better.
Even healthcare professionals such as Dr Deepak Ravindran, who is a consultant at the Royal Berkshire NHS Foundation Trust, are looking towards patients such as Louise or Tim for guidance away from outdated approaches.
He said: "It helps to make patients believe that there can be other ways of relieving pain and indeed sometimes “curing” pain without resorting to biomedical approaches of more tablets or more interventions."
Combining both medical advice and the nuance of the lived experience is also crucial for Mr Ravindran and his practices - "If we are to provide a value based health care, then we need to first understand what matters most to the patient and what is of greatest value to them when we are trying to provide pain relief."
A modern day understanding of pain is less focussed on opioids and medication. Now, it's focussed on empowering the patient who has had the lived experience to not be completely crippled by it.


